Healthy Body
|
|
Staff
It’s that time of year. Spring has arrived, and summer is just around the corner! What does this mean? Sleeveless tops, sandals, capris…and, yes…bathing suits, ladies. Basically, along with the warm weather comes clothing that exposes more of our skin.
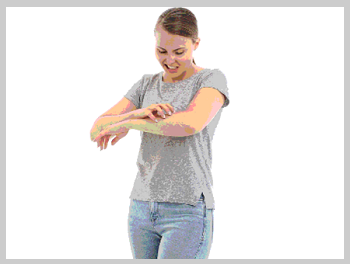
On top of making sure we don’t miss our next Pilates or spin class, we want to also be sure our skin looks clear and healthy. Those of us with skin conditions, such as eczema, begin to dread this inevitable exposure and seek to find ways to control the flare-ups.
According to the American College of Allergy, Asthma & Immunology, “Although most people associate the development of eczema in childhood, it can also appear [later in life]. The condition seems to be more common in urban areas and developed countries and affects men and women of all races equally. Eczema is not contagious. You or your child cannot “catch” it from another person or give it to someone else.”
It’s that time of year. Spring has arrived, and summer is just around the corner! What does this mean? Sleeveless tops, sandals, capris…and, yes…bathing suits, ladies. Basically, along with the warm weather comes clothing that exposes more of our skin.
On top of making sure we don’t miss our next Pilates or spin class, we want to also be sure our skin looks clear and healthy. Those of us with skin conditions, such as eczema, begin to dread this inevitable exposure and seek to find ways to control the flare-ups.
According to the American College of Allergy, Asthma & Immunology, “Although most people associate the development of eczema in childhood, it can also appear [later in life]. The condition seems to be more common in urban areas and developed countries and affects men and women of all races equally. Eczema is not contagious. You or your child cannot “catch” it from another person or give it to someone else.”
Nevertheless, good sleep, fulfilling activities, close relationships, and positive self-esteem can be casualties of atopic dermatitis, the chronic skin condition often called “eczema.”
“We’ve seen rates of atopic dermatitis – or ‘AD’ – climb,” notes Angie Seelal, R-PAC, specializing in dermatology with Advanced Dermatology PC. “A growing number of people can benefit from interventions to manage this disruptive skin condition.”
Atopic dermatitis usually starts at a young age, most often under five. Dry, scaly, red patches of skin develop, often on the face, arms or legs. “These affected areas are extremely itchy,” explains Seelal, “interfering with sleep and triggering scratching that can bring additional skin problems: worsened inflammation and the risk of infection.”
Following the first occurrence, symptoms may subside and flare up. About half will see symptoms cease completely by adulthood. For others, the red, itchy patches can continue.
Since the 1970s, AD cases have increased, with some industrialized countries’ numbers tripling. “Research has yet to fully identify why,” says Seelal, “but in the U.S., about 9.6 million of those under eighteen have AD, and more than 16 million adults are dealing with the condition.”
Atopic dermatitis is not contagious, despite its appearance. Research points to a confluence of genes and environment that trigger an immune system misfire. Genetically, there is a connection between AD, asthma and hay fever; parents with any one of these ailments are more likely to have children who develop AD. “Research has also focused on the skin protein ‘filaggrin,’ which helps maintain a protective skin barrier,” Seelal reports. “A mutation in the gene that codes for filaggrin may be implicated in AD.”
At this point, there is no cure for AD. “But we have effective treatments that can help patients control symptoms. And early treatment can ward off long-term damage, like lichenification – skin thickening that can result from chronic scratching,” Seelal emphasizes.
To help patients manage AD, Seelal suggests the following:
Six Tips to Help Control Atopic Dermatitis
1. Moisturize, Moisturize, Moisturize: “Dry skin is the enemy,” warns Seelal, “and we also want to build up the skin’s protective barrier. With AD, a super-effective moisturizer is needed. Ointments’ higher oil content provides the most protection. People should avoid any additives that may be irritants, so it's imperative to consult your dermatologist. Also, the National Eczema Association’s website has a list of evaluated products. Do a trial run on a small spot to check for sensitivity. Your moisturizer should be handy at every household sink for post-washing and packaged to go for re-application when out and about.”
2. Bathe Smart: “An effective bath or shower routine helps us maximize moisturizing,” explains Seelal. “‘Effective’ means lukewarm water instead of hot, using a gentle cleanser for sensitive skin, and staying away from scrubbing and soap. Then, we’re set up for moisturizing.”
3. Follow the Three-Minute Rule: “After washing, “we’re primed to moisturize, but we need to do this in a timely way,” cautions Seelal. “An oil-rich moisturizer should be applied within three minutes to seal in moisture. If we have topical medications, those should be applied first, followed by the moisturizer.”
4. Options for Topical Treatments: “Moisturizing is required,” Seelal points out. “But often it’s not enough. Corticosteroids, topical calcineurin inhibitors (TCIs), and PDE4 inhibitors are topical treatments with different mechanisms for tamping down the body’s immune response to decrease inflammation. Patients should talk with their doctor to get a clear understanding of how each medicine works and to learn about its side effects. Steroidal treatment, for example, is often limited, while TCIs may be long-term.”
5. Light Therapy Requires Commitment: “Phototherapy – most often in the form of UVB rays – can help up to 70 percent of patients who haven’t improved with topical treatment,” notes Seelal. “But it involves frequent ongoing treatments.”
6. Learn about Targeted ‘Biologic’ Treatment: “In 2017, the FDA approved Dupixent® as the first ‘biologic’ drug for AD,” Seelal reports. “It works on a genetic level to block proteins that trigger skin inflammation. Patients receive every-other-week injections.”
Be sure to work with your healthcare provider to come up with a plan that will work for you.
“Your dermatologist can help customize a plan so that AD doesn’t devastate your life,” Sellal adds.
“We’ve seen rates of atopic dermatitis – or ‘AD’ – climb,” notes Angie Seelal, R-PAC, specializing in dermatology with Advanced Dermatology PC. “A growing number of people can benefit from interventions to manage this disruptive skin condition.”
Atopic dermatitis usually starts at a young age, most often under five. Dry, scaly, red patches of skin develop, often on the face, arms or legs. “These affected areas are extremely itchy,” explains Seelal, “interfering with sleep and triggering scratching that can bring additional skin problems: worsened inflammation and the risk of infection.”
Following the first occurrence, symptoms may subside and flare up. About half will see symptoms cease completely by adulthood. For others, the red, itchy patches can continue.
Since the 1970s, AD cases have increased, with some industrialized countries’ numbers tripling. “Research has yet to fully identify why,” says Seelal, “but in the U.S., about 9.6 million of those under eighteen have AD, and more than 16 million adults are dealing with the condition.”
Atopic dermatitis is not contagious, despite its appearance. Research points to a confluence of genes and environment that trigger an immune system misfire. Genetically, there is a connection between AD, asthma and hay fever; parents with any one of these ailments are more likely to have children who develop AD. “Research has also focused on the skin protein ‘filaggrin,’ which helps maintain a protective skin barrier,” Seelal reports. “A mutation in the gene that codes for filaggrin may be implicated in AD.”
At this point, there is no cure for AD. “But we have effective treatments that can help patients control symptoms. And early treatment can ward off long-term damage, like lichenification – skin thickening that can result from chronic scratching,” Seelal emphasizes.
To help patients manage AD, Seelal suggests the following:
Six Tips to Help Control Atopic Dermatitis
1. Moisturize, Moisturize, Moisturize: “Dry skin is the enemy,” warns Seelal, “and we also want to build up the skin’s protective barrier. With AD, a super-effective moisturizer is needed. Ointments’ higher oil content provides the most protection. People should avoid any additives that may be irritants, so it's imperative to consult your dermatologist. Also, the National Eczema Association’s website has a list of evaluated products. Do a trial run on a small spot to check for sensitivity. Your moisturizer should be handy at every household sink for post-washing and packaged to go for re-application when out and about.”
2. Bathe Smart: “An effective bath or shower routine helps us maximize moisturizing,” explains Seelal. “‘Effective’ means lukewarm water instead of hot, using a gentle cleanser for sensitive skin, and staying away from scrubbing and soap. Then, we’re set up for moisturizing.”
3. Follow the Three-Minute Rule: “After washing, “we’re primed to moisturize, but we need to do this in a timely way,” cautions Seelal. “An oil-rich moisturizer should be applied within three minutes to seal in moisture. If we have topical medications, those should be applied first, followed by the moisturizer.”
4. Options for Topical Treatments: “Moisturizing is required,” Seelal points out. “But often it’s not enough. Corticosteroids, topical calcineurin inhibitors (TCIs), and PDE4 inhibitors are topical treatments with different mechanisms for tamping down the body’s immune response to decrease inflammation. Patients should talk with their doctor to get a clear understanding of how each medicine works and to learn about its side effects. Steroidal treatment, for example, is often limited, while TCIs may be long-term.”
5. Light Therapy Requires Commitment: “Phototherapy – most often in the form of UVB rays – can help up to 70 percent of patients who haven’t improved with topical treatment,” notes Seelal. “But it involves frequent ongoing treatments.”
6. Learn about Targeted ‘Biologic’ Treatment: “In 2017, the FDA approved Dupixent® as the first ‘biologic’ drug for AD,” Seelal reports. “It works on a genetic level to block proteins that trigger skin inflammation. Patients receive every-other-week injections.”
Be sure to work with your healthcare provider to come up with a plan that will work for you.
“Your dermatologist can help customize a plan so that AD doesn’t devastate your life,” Sellal adds.
Angie Seelal, RPA-C, is a Certified Physician Assistant through the National Commission of Certification of Physician Assistants who specializes in dermatology and is a member of many prestigious associations, including American Academy of Physician Assistants, the National Psoriasis Foundation, the Society of Dermatology Physician Assistants, and New York State Society of Physician Assistants. In 2012, she joined Advanced Dermatology P.C., a leading dermatology center, offering highly experienced physicians in the fields of cosmetic and laser dermatology as well as plastic surgery and state-of-the-art medical technologies.